


生物技术进展 ›› 2023, Vol. 13 ›› Issue (4): 524-533.DOI: 10.19586/j.2095-2341.2023.0025
• 进展评述 • 上一篇
李世明1,2( ), 张鹏3, 赵鹏翔1, 谢飞1, 陈晓萍2(
), 张鹏3, 赵鹏翔1, 谢飞1, 陈晓萍2( ), 刘梦昱1(
), 刘梦昱1( )
)
收稿日期:2023-03-01
接受日期:2023-04-11
出版日期:2023-07-25
发布日期:2023-08-03
通讯作者:
陈晓萍,刘梦昱
作者简介:李世明 E-mail: 1317907921@qq.com;
基金资助:
Shiming LI1,2( ), Peng ZHANG3, Pengxiang ZHAO1, Fei XIE1, Xiaoping CHEN2(
), Peng ZHANG3, Pengxiang ZHAO1, Fei XIE1, Xiaoping CHEN2( ), Mengyu LIU1(
), Mengyu LIU1( )
)
Received:2023-03-01
Accepted:2023-04-11
Online:2023-07-25
Published:2023-08-03
Contact:
Xiaoping CHEN,Mengyu LIU
摘要:
骨骼肌具有高度可塑性,可根据功能需求发生改变。活动水平的降低或停用,通常会导致肌萎缩和代谢功能障碍。因肌肉负荷急剧下降和神经激活受到抑制而导致的骨骼肌质量损失,通常被称为废用性肌萎缩。骨骼肌的收缩活性、高耗氧量和代谢使其持续产生适量的氧化物质,如活性氧(reactive oxygen species,ROS)。当氧化产物超过抗氧化防御能力时,机体就会进入氧化应激状态。在骨骼肌长期停用期间,氧化应激至少通过3种方式增加蛋白质的降解,或在起始水平阻碍mRNA翻译抑制蛋白质合成,从而促进骨骼肌萎缩。随着我国航天事业的迅速发展,失重状态下的废用性肌萎缩也是航天医学亟待解决的问题。概述了废用性肌萎缩以及氧化应激在废用性肌萎缩中的作用,以期为废用性肌萎缩的临床治疗与实践提供有价值的参考。
中图分类号:
李世明, 张鹏, 赵鹏翔, 谢飞, 陈晓萍, 刘梦昱. 氧化应激与废用性肌萎缩研究进展[J]. 生物技术进展, 2023, 13(4): 524-533.
Shiming LI, Peng ZHANG, Pengxiang ZHAO, Fei XIE, Xiaoping CHEN, Mengyu LIU. Research Progress of Oxidative Stress and Disuse Muscular Atrophy[J]. Current Biotechnology, 2023, 13(4): 524-533.
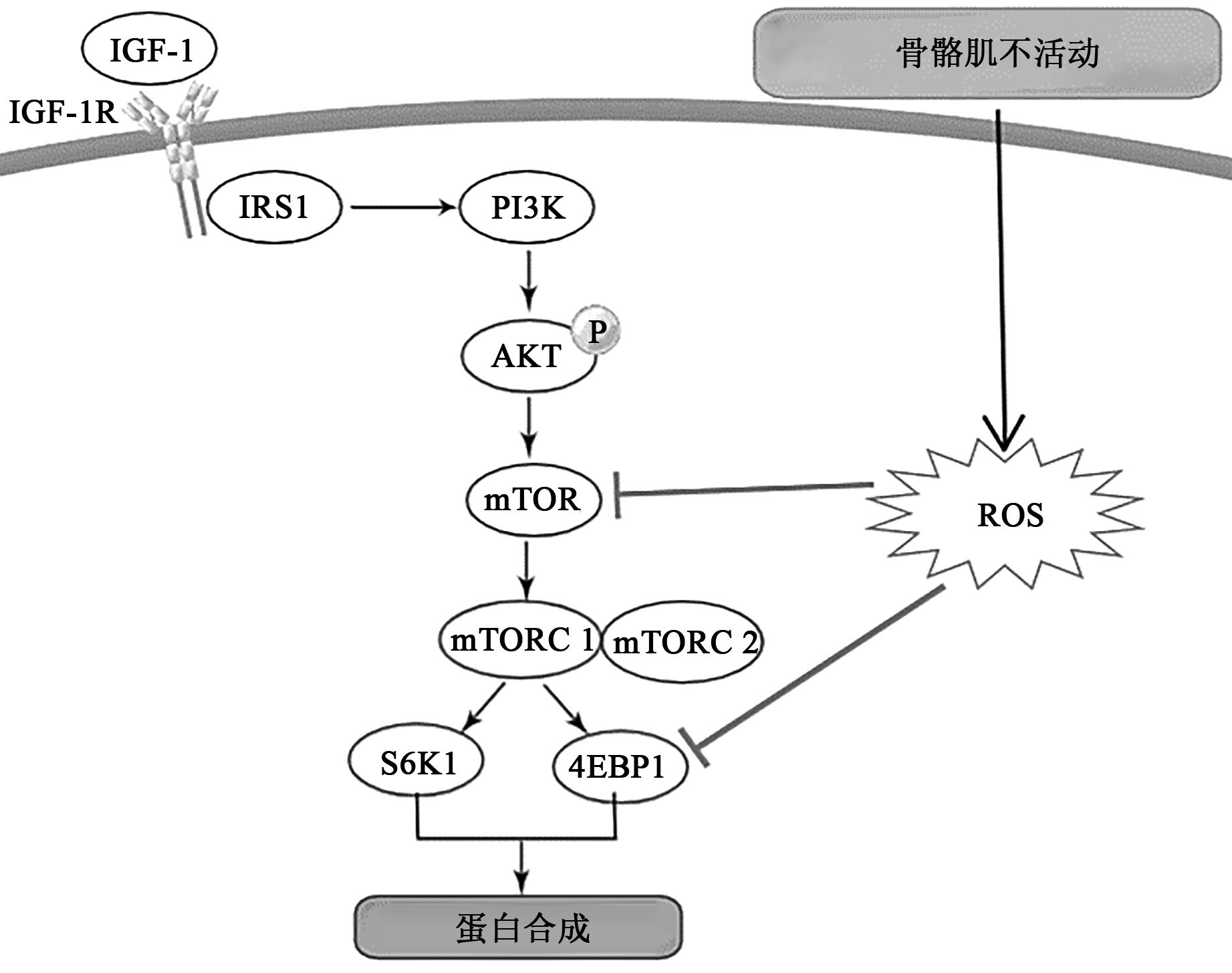
图2 氧化应激抑制骨骼肌蛋白质合成的主要方式注:IGF-1—胰岛素样生长因子1;IGF-1R—胰岛素样生长因子1受体;IRS1—胰岛素受体底物1;PI3K—磷脂酰肌醇-3激酶;AKT—蛋白激酶B;mTOR—雷帕霉素哺乳动物靶标;S6K1—蛋白激酶1;4EBP1—真核翻译起始因子-4E结合蛋白1。
Fig. 2 Major ways in which oxidative stress inhibits skeletal muscle protein synthesis
| 1 | MUKUND K, SUBRAMANIAM S. Skeletal muscle: a review of molecular structure and function, in health and disease[J/OL]. WIRES Syst. Biol. Med., 2020, 12(1): e1462[2019-08-14]. . |
| 2 | NUNES E A, STOKES T, MCKENDRY J, et al.. Disuse-induced skeletal muscle atrophy in disease and nondisease states in humans: mechanisms, prevention, and recovery strategies[J]. Am. J. Physiol. Cell Physiol., 2022, 322(6): 1068-1084. |
| 3 | FUKADA S I. The roles of muscle stem cells in muscle injury, atrophy and hypertrophy[J]. J. Biochem., 2018, 163(5): 353-358. |
| 4 | YIN L, LI N, JIA W, et al.. Skeletal muscle atrophy: from mechanisms to treatments[J]. Pharmacol. Res., 2021, 172: 105807[2021-08-10]. . |
| 5 | DUAN K, GAO X, ZHU D. The clinical relevance and mechanism of skeletal muscle wasting[J]. Clin. Nutr., 2021, 40(1): 27-37. |
| 6 | CHEMELLO F, BEAN C, CANCELLARA P, et al.. Microgenomic analysis in skeletal muscle: expression signatures of individual fast and slow myofibers[J/OL]. PLoS ONE, 2011, 6(2): e16807[2011-02-22]. . |
| 7 | ZHOU J, LIU B, LIANG C, et al.. Cytokine signaling in skeletal muscle wasting[J]. Trends Endocrinol. Metab., 2016, 27(5): 335-347. |
| 8 | SZENTESI P, CSERNOCH L, DUX L, et al.. Changes in redox signaling in the skeletal muscle with aging[J/OL]. Oxid. Med. Cell Longev., 2019, 2019: 4617801[2019-01-17]. . |
| 9 | HAFEN P S, ABBOTT K, BOWDEN J, et al.. Daily heat treatment maintains mitochondrial function and attenuates atrophy in human skeletal muscle subjected to immobilization[J]. J. Appl. Physiol., 2019, 127(1): 47-57. |
| 10 | HYATT H, DEMINICE R, YOSHIHARA T, et al.. Mitochondrial dysfunction induces muscle atrophy during prolonged inactivity: a review of the causes and effects[J]. Arch. Biochem. Biophys., 2019, 662: 49-60. |
| 11 | MULLER F L, SONG W, JANG Y C, et al.. Denervation-induced skeletal muscle atrophy is associated with increased mitochondrial ROS production[J]. Am. J. Physiol. Regul. Integr. Comp. Physiol., 2007, 293(3): 1159-1168. |
| 12 | HUANG M Z, LI J Y. Physiological regulation of reactive oxygen species in organisms based on their physicochemical properties[J/OL]. Acta Physiol., 2020, 228(1): e13351[2019-07-25]. . |
| 13 | MEO S D, NAPOLITANO G, VENDITTI P. Mediators of physical activity protection against ROS-linked skeletal muscle damage[J/OL]. Int. J. Mol. Sci., 2019, 20(12): 3024[2019-06-20]. . |
| 14 | BOUVIERE J, FORTUNATO R S, DUPUY C, et al.. Exercise-stimulated ROS sensitive signaling pathways in skeletal muscle[J/OL]. Antioxidants, 2021, 10(4):537[2021-03-30]. . |
| 15 | MAKHNOVSKII P A, ZGODA V G, BOKOV R O, et al.. Regulation of proteins in human skeletal muscle: the role of transcription[J/OL]. Sci. Rep., 2020, 10(1): 3514[2020-02-26]. . |
| 16 | HUANG L, LI M, DENG C, et al.. Potential therapeutic strategies for skeletal muscle atrophy[J/OL]. Antioxidants, 2022, 12(1):44[2022-12-26]. . |
| 17 | MALAVAKI C J, SAKKAS G K, MITROU G I, et al.. Skeletal muscle atrophy: disease-induced mechanisms may mask disuse atrophy[J]. J. Muscle Res. Cell Motil., 2015, 36(6): 405-421. |
| 18 | JUN L, ROBINSON M, GEETHA T, et al.. Prevalence and mechanisms of skeletal muscle atrophy in metabolic conditions[J/OL]. Int. J. Mol. Sci., 2023, 24(3): 2973[2023-02-03]. . |
| 19 | CANEPARI M, PELLEGRINO M A, D'ANTONA G, et al.. Skeletal muscle fibre diversity and the underlying mechanisms[J]. Acta Physiol., 2010, 199(4): 465-476. |
| 20 | FITTS R H, TRAPPE S W, COSTILL D L, et al.. Prolonged space flight-induced alterations in the structure and function of human skeletal muscle fibres[J]. J. Physiol., 2010, 588(18): 3567-3592. |
| 21 | AOI W, TAKANAMI Y, KAWAI Y, et al.. Contribution of oxidative stress to protein catabolism in skeletal muscle[J/OL]. Med. Sci. Phys. Exerc., 2007, 39(5): S313[2007-05-31]. . |
| 22 | PARKER E, KHAYRULLIN A, KENT A, et al.. Hindlimb immobilization increases IL-1β and Cdkn2a expression in skeletal muscle fibro-adipogenic progenitor cells: a link between senescence and muscle disuse atrophy[J/OL]. Front. Cell Dev. Biol., 2021, 9: 790437[2022-01-03]. . |
| 23 | ELEY H L, TISDALE M J. Skeletal muscle atrophy, a link between depression of protein synthesis and increase in degradation[J]. J. Biol. Chem., 2007, 282(10): 7087-7097. |
| 24 | POMATTO L C D, DAVIES K J A. Adaptive homeostasis and the free radical theory of ageing[J]. Free Radic. Biol. Med., 2018, 124: 420-430. |
| 25 | SOHAL R S, MOCKETT R J, ORR W C. Mechanisms of aging: an appraisal of the oxidative stress hypothesis[J]. Free Radic. Biol. Med., 2002, 33(5): 575-586. |
| 26 | BURTON G J, JAUNIAUX E. Oxidative stress[J]. Best Pract. Res. Clin. Obstet. Gynaecol., 2011, 25(3): 287-299. |
| 27 | KONDO H, MIURA M, ITOKAWA Y. Oxidative stress in skeletal muscle atrophied by immobilization[J]. Acta Physiol. Scand., 1991, 142(4): 527-528. |
| 28 | POWERS S K, KAVAZIS A N, MCCLUNG J M. Oxidative stress and disuse muscle atrophy[J]. J. Appl. Physiol. 2007, 102(6): 2389-2397. |
| 29 | POWERS S K, OZDEMIR M, HYATT H. Redox control of proteolysis during inactivity-induced skeletal muscle atrophy[J]. Antioxid. Redox Sign., 2020, 33(8): 559-569. |
| 30 | POWERS S K, WIGGS M P, DUARTE J A, et al.. Mitochondrial signaling contributes to disuse muscle atrophy[J]. Am. J. Physiol. Endocrinol. Metab., 2012, 303(1): 31-39. |
| 31 | KAVAZIS A N, TALBERT E E, SMUDER A J, et al.. Mechanical ventilation induces diaphragmatic mitochondrial dysfunction and increased oxidant production[J]. Free Radic. Biol. Med., 2009, 46(6): 842-850. |
| 32 | TALBERT E E, SMUDER A J, MIN K, et al.. Immobilization-induced activation of key proteolytic systems in skeletal muscles is prevented by a mitochondria-targeted antioxidant[J]. J. Appl. Physiol., 2013, 115(4): 529-538. |
| 33 | LARSEN S, DANDANELL S, KRISTENSEN K B, et al.. Influence of exercise amount and intensity on long-term weight loss maintenance and skeletal muscle mitochondrial ROS production in humans[J]. Appl. Physiol. Nutr. Me., 2019, 44(9): 958-964. |
| 34 | POWERS S K. Can antioxidants protect against disuse muscle atrophy?[J/OL]. Sports Med., 2014, 44 (S2): 155-165: 3024[2019-06-20].. |
| 35 | MEO S D, NAPOLITANO G, VENDITTI P. Mediators of physical activity protection against ROS-linked skeletal muscle damage[J]. Int. J. Mol. Sci., 2019, 20(12): 3024[2019-06-20].. |
| 36 | DRES M, DEMOULE A. Diaphragm dysfunction during weaning from mechanical ventilation: an underestimated phenomenon with clinical implications[J/OL]. Crit. Care, 2018, 22(1): 73[2018-03-20]. . |
| 37 | RODNEY G G, PAL R, ABO-ZAHRAH R. Redox regulation of autophagy in skeletal muscle[J]. Free Radic. Biol. Med., 2016, 98: 103-112. |
| 38 | WILLIAMSON J, DAVISON G. Targeted antioxidants in exercise-Induced mitochondrial oxidative stress: emphasis on DNA damage[J/OL]. Antioxidants, 2020, 9(11):1142[2020-11-17]. . |
| 39 | VELJKOVIĆ A, HADŽI-DOKIĆ J, SOKOLOVIĆ D, et al.. Xanthine oxidase/dehydrogenase activity as a source of oxidative stress in prostate cancer tissue[J/OL]. Diagnostics, 2020, 10(9):668[2020-09-03]. . |
| 40 | FERREIRA L F, LAITANO O. Regulation of NADPH oxidases in skeletal muscle[J]. Free Radic. Biol Med., 2016, 98: 18-28. |
| 41 | MIN K, SMUDER A J, KWON O S, et al.. Mitochondrial-targeted antioxidants protect skeletal muscle against immobilization-induced muscle atrophy[J]. J. Appl. Physiol., 2011, 111(5): 1459-1466. |
| 42 | FALK D J, KAVAZIS A N, WHIDDEN M A, et al.. Mechanical ventilation-induced oxidative stress in the diaphragm: role of heme oxygenase-1[J]. Chest, 2011, 139(4): 816-824. |
| 43 | MCCLUNG J M, VAN GAMMEREN D, WHIDDEN M A, et al.. Apocynin attenuates diaphragm oxidative stress and protease activation during prolonged mechanical ventilation[J]. Crit. Care Med., 2009, 37(4): 1373-1379. |
| 44 | WHIDDEN M A, MCCLUNG J M, FALK D J, et al.. Xanthine oxidase contributes to mechanical ventilation-induced diaphragmatic oxidative stress and contractile dysfunction[J]. J. Appl. Physiol., 2009, 106(2): 385-394. |
| 45 | WHIDDEN M A, SMUDER A J, WU M, et al.. Oxidative stress is required for mechanical ventilation-induced protease activation in the diaphragm[J]. J. Appl. Physiol., 2010, 108(5): 1376-1382. |
| 46 | SHANELY R A, ZERGEROGLU M A, LENNON S L, et al.. Mechanical ventilation-induced diaphragmatic atrophy is associated with oxidative injury and increased proteolytic activity[J]. Am. J. Resp. Crit. Care Med., 2002, 166(10): 1369-1374. |
| 47 | POWERS S K, HUDSON M B, NELSON W B, et al.. Mitochondria-targeted antioxidants protect against mechanical ventilation-induced diaphragm weakness[J]. Crit. Care Med., 2011, 39(7): 1749-1759. |
| 48 | POWERS S K, SMUDER A J, CRISWELL D S. Mechanistic links between oxidative stress and disuse muscle atrophy[J]. Antioxid Redox Sign., 2011, 15(9): 2519-2528. |
| 49 | MEBRATU Y A, NEGASI Z H, DUTTA S, et al.. Adaptation of proteasomes and lysosomes to cellular environments[J/OL]. Cells, 2020, 9(10): 2221[2020-10-01]. . |
| 50 | MARGETA M. Autophagy defects in skeletal myopathies[J]. Annu. Rev. Pathol., 2020, 15: 261-285. |
| 51 | GE L, XU Y, XIA W, et al.. Synergistic action of cathepsin B, L, D and calpain in disassembly and degradation of myofibrillar protein of grass carp[J]. Food Res. Int., 2018, 109: 481-488. |
| 52 | MAMMUCARI C, MILAN G, ROMANELLO V, et al.. FoxO3 controls autophagy in skeletal muscle in vivo [J]. Cell Metab., 2007, 6(6): 458-471. |
| 53 | HYATT H W, OZDEMIR M, YOSHIHARA T, et al.. Calpains play an essential role in mechanical ventilation-induced diaphragmatic weakness and mitochondrial dysfunction[J/OL]. Redox Biol., 2021, 38: 101802[2020-11-25]. . |
| 54 | SMUDER A J, SOLLANEK K J, NELSON W B, et al.. Crosstalk between autophagy and oxidative stress regulates proteolysis in the diaphragm during mechanical ventilation[J]. Free Radic. Biol. Med., 2018, 115: 179-190. |
| 55 | NAVARRO-YEPES J, BURNS M, ANANDHAN A, et al.. Oxidative stress, redox signaling, and autophagy: cell death versus survival [J]. Antioxid. Redox Sign., 2014, 21(1): 66-85. |
| 56 | WANG J, SUN L, LI X, et al.. Alkali exposure induces autophagy through activation of the MAPK pathway by ROS and inhibition of mTOR in Eriocheir sinensis [J]. Aquat. Toxicol., 2023, 258: 106481[2023-03-09]. . |
| 57 | ZHUANG Y, LI Y, LI X, et al.. Atg7 knockdown augments concanavalin A-induced acute hepatitis through an ROS-mediated p38/MAPK pathway[J/OL]. PLoS ONE, 2016, 11(3): e0149754[2016-03-03]. . |
| 58 | NGUYEN T N, PADMAN B S, USHER J, et al.. Atg8 family LC3/GABARAP proteins are crucial for autophagosome-lysosome fusion but not autophagosome formation during PINK1/Parkin mitophagy and starvation[J]. J. Cell Biol., 2016, 215(6): 857-874. |
| 59 | MØLLER A B, VENDELBO M H, SCHJERLING P, et al.. Immobilization decreases FOXO3a phosphorylation and increases autophagy-related gene and protein expression in human skeletal muscle[J/OL]. Front. Physiol., 2019, 10: 736[2019-06-14]. . |
| 60 | FÖRSTER F, LASKER K, BECK F, et al.. An atomic model AAA-ATPase/20S core particle sub-complex of the 26S proteasome[J]. Biochem. Biophys. Res. Commun., 2009, 388(2): 228-233. |
| 61 | TUREK I, TISCHER N, LASSIG R, et al.. Multi-tiered pairing selectivity between E2 ubiquitin-conjugating enzymes and E3 ligases[J]. J. Biol. Chem., 2018, 293(42): 16324-16336. |
| 62 | BODINE S C, BAEHR L M. Skeletal muscle atrophy and the E3 ubiquitin ligases MuRF1 and MAFbx/atrogin-1[J]. Am. J. Physiol. Endocrinol. Metab., 2014, 307(6): 469-484. |
| 63 | KOROVILA I, HUGO M, CASTRO J P, et al.. Proteostasis, oxidative stress and aging[J]. Redox Biol., 2017, 13: 550-567. |
| 64 | LEFAKI M, PAPAEVGENIOU N, CHONDROGIANNI N. Redox regulation of proteasome function[J]. Redox Biol., 2017, 13: 452-458. |
| 65 | LI Y P, CHEN Y, LI A S, et al.. Hydrogen peroxide stimulates ubiquitin-conjugating activity and expression of genes for specific E2 and E3 proteins in skeletal muscle myotubes[J]. Am. J. Physiol. Cell Physiol., 2003, 285(4): 806-812. |
| 66 | KIM J, PARK H, SARAVANAKUMAR G, et al.. Polymer/aptamer-integrated gold nanoconstruct suppresses the inflammatory process by scavenging ROS and capturing pro-inflammatory cytokine TNF-α[J]. ACS Appl. Mater. Interfaces, 2021, 13(8): 9390-9401. |
| 67 | HYATT H W, POWERS S K. The role of calpains in skeletal muscle remodeling with exercise and inactivity-induced atrophy[J]. Int. J. Sports Med., 2020, 41(14): 994-1008. |
| 68 | PIERRE N, BARBÉ C, GILSON H, et al.. Activation of ER stress by hydrogen peroxide in C2C12 myotubes[J]. Biochem. Biophys. Res. Commun., 2014, 450(1): 459-463. |
| 69 | DARGELOS E, BRULÉ C, STUELSATZ P, et al.. Up-regulation of calcium-dependent proteolysis in human myoblasts under acute oxidative stress[J]. Exp. Cell Res., 2010, 316(1): 115-125. |
| 70 | MAHARJAN S, SAKAI Y, HOSEKI J. Screening of dietary antioxidants against mitochondria-mediated oxidative stress by visualization of intracellular redox state[J]. Biosci. Biotechnol. Biochem., 2016, 80(4): 726-734. |
| 71 | ZHU X, VAN HEES H W H, HEUNKS L, et al.. The role of calpains in ventilator-induced diaphragm atrophy[J/OL]. Intens. Care Med. Exp, 2017, 5(1): 14[2017-03-14].. |
| 72 | HYATT H W, OZDEMIR M, BOMKAMP M P, et al.. Activation of calpain contributes to mechanical ventilation-induced depression of protein synthesis in diaphragm muscle[J/OL]. Cells, 2022, 11(6): 1028[2022-03-18].. |
| 73 | FANG X, WU C, LI H, et al.. Elevation of intracellular calcium and oxidative stress is involved in perfluorononanoic acid-induced neurotoxicity[J]. Toxicol. Ind. Health, 2018, 34(3): 139-145. |
| 74 | GOLL D E, THOMPSON V F, LI H, et al.. The calpain system[J]. Physiol. Rev., 2003, 83(3): 731-801. |
| 75 | ANDERSSON D C, BETZENHAUSER M J, REIKEN S, et al.. Ryanodine receptor oxidation causes intracellular calcium leak and muscle weakness in aging[J]. Cell Metab., 2011, 14(2): 196-207. |
| 76 | SMUDER A J, KAVAZIS A N, HUDSON M B, et al.. Oxidation enhances myofibrillar protein degradation via calpain and caspase-3[J]. Free Radic. Biol. Med., 2010, 49(7): 1152-1160. |
| 77 | MCCLUNG J M, KAVAZIS A N, DERUISSEAU K C, et al.. Caspase-3 regulation of diaphragm myonuclear domain during mechanical ventilation-induced atrophy[J]. Am. J. Respir. Crit. Care Med., 2007, 175(2): 150-159. |
| 78 | HUANG F, HUANG M, ZHOU G, et al.. In vitro proteolysis of myofibrillar proteins from beef skeletal muscle by caspase-3 and caspase-6[J]. J. Agric. Food Chem., 2011, 59(17): 9658-9663. |
| 79 | POWERS S K, KAVAZIS A N, DERUISSEAU K C. Mechanisms of disuse muscle atrophy: role of oxidative stress[J]. Am. J. Physiol. Regul. Integr. Comp. Physiol., 2005, 288(2): 337-344. |
| 80 | DAVIES K J. Protein damage and degradation by oxygen radicals. I. general aspects[J]. J. Biol. Chem., 1987, 262(20): 9895-9901. |
| 81 | RAYNES R, POMATTO L C D, DAVIES K J A. Degradation of oxidized proteins by the proteasome: distinguishing between the 20S, 26S, and immunoproteasome proteolytic pathways[J]. Mol. Aspects Med., 2016, 50: 41-55. |
| 82 | YUAN Z M, LI M, JI C Y, et al.. Steady hydrodynamic interaction between human swimmers[J/OL]. J. R. Soc. Interface, 2019, 16(150): 20180768[2019-01-23]. . |
| 83 | KIM A Y, SEO J B, KIM W T, et al.. The pathogenic human Torsin A in Drosophila activates the unfolded protein response and increases susceptibility to oxidative stress[J/OL]. BMC Genom., 2015, 16(1): 338[2015-04-23].. |
| 84 | POWERS S K, MORTON A B, AHN B, et al. Redox control of skeletal muscle atrophy[J]. Free Radic. Biol. Med., 2016, 98: 208-217. |
| 85 | TAN P L, SHAVLAKADZE T, GROUNDS M D, et al.. Differential thiol oxidation of the signaling proteins Akt, PTEN or PP2A determines whether Akt phosphorylation is enhanced or inhibited by oxidative stress in C2C12 myotubes derived from skeletal muscle[J]. Int. J. Biochem. Cell Biol., 2015, 62: 72-79. |
| 86 | ERDMANN-PHAM D D, DUC K D, SONG Y S. The key parameters that govern translation efficiency[J]. Cell Syst., 2020, 10(2): 183-192. |
| 87 | MERRICK W C. eIF4F: a retrospective[J]. J. Biol. Chem., 2015, 290(40): 24091-24099. |
| 88 | MODRAK-WOJCIK A, GORKA M, NIEDZWIECKA K, et al.. Eukaryotic translation initiation is controlled by cooperativity effects within ternary complexes of 4E-BP1, eIF4E, and the mRNA 5' cap[J]. FEBS Lett., 2013, 587(24): 3928-3934. |
| 89 | BÖHM R, IMSENG S, JAKOB R P, et al.. The dynamic mechanism of 4E-BP1 recognition and phosphorylation by mTORC1[J]. Mol. Cell, 2021, 81(11): 2403-2416. |
| 90 | SUN R, CHENG E, VELÁSQUEZ C, et al.. Mitosis-related phosphorylation of the eukaryotic translation suppressor 4E-BP1 and its interaction with eukaryotic translation initiation factor 4E (eIF4E)[J]. J. Biol. Chem., 2019, 294(31): 11840-11852. |
| 91 | PHAM F H, SUGDEN P H, CLERK A. Regulation of protein kinase B and 4E-BP1 by oxidative stress in cardiac myocytes[J]. Circ. Res., 2000, 86(12): 1252-1258. |
| 92 | QIU Z, WANG L, MAO H, et al.. miR-370 inhibits the oxidative stress and apoptosis of cardiac myocytes induced by hydrogen peroxide by targeting FOXO1[J]. Exp. Ther. Med., 2019, 18(4): 3025-3031. |
| 93 | HUDSON M B, SMUDER A J, NELSON W B, et al.. Partial support ventilation and mitochondrial-targeted antioxidants protect against ventilator-induced decreases in diaphragm muscle protein synthesis[J/OL]. PLoS ONE, 2015, 10(9): e0137693[2015-09-11]. . |
| [1] | 曹丽, 罗顺, 邢世海, 仇金树, 蔺智勇, 林军, 孟旭, 刘峰. 山药提取物对CHO细胞生长及抗体表达的影响[J]. 生物技术进展, 2023, 13(3): 449-456. |
| [2] | 曹静钰, 刘承梅, 祁晨旭, 杜开颜, 陈蒙, 侯思伟. Nrf2在脊髓损伤后铁死亡的研究进展[J]. 生物技术进展, 2023, 13(2): 240-246. |
| [3] | 陈军, 秦树存, 何磊. 富氢盐水对咪喹莫特诱导小鼠银屑病的抑制作用[J]. 生物技术进展, 2022, 12(4): 503-509. |
| [4] | 王珍,杨洛,廖敏,郝亚荣. mTOR信号通路在糖尿病肾病发病机制中的研究进展[J]. 生物技术进展, 2021, 11(3): 316-321. |
| [5] | 赵杰,张伟杰,陈瑶,项清芳,赵婷,茆广华,冯伟伟,仰榴青. 蜂蛹多肽对巨噬细胞RAW264.7免疫活性的影响[J]. 生物技术进展, 2020, 10(5): 550-556. |
| [6] | 熊咏民,杨晓莉,张荣强,李宝荣,陈静宏,代晓霞,陈群,谭武红,张峰. 硒在地方病中的防治作用及其分子机制研究进展[J]. 生物技术进展, 2017, 7(5): 501-505. |
| [7] | 杨玉洁,李楠. 硒蛋白与神经退行性疾病[J]. 生物技术进展, 2017, 7(5): 511-517. |
| [8] | 李佳腊,张亚婷,谢飞. 氢分子在癌症防治中的应用进展[J]. 生物技术进展, 2016, 6(3): 174-178. |
| [9] | 赵忠朝,张玉秀,周正富,张维,陈明. 耐辐射异常球菌抗氧化保护机制的研究进展[J]. 生物技术进展, 2013, 3(2): 109-114. |
| [10] | 张怡,路铁刚. 植物中的活性氧研究概述[J]. 生物技术进展, 2011, 1(4): 242-248. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||
版权所有 © 2021《生物技术进展》编辑部